-
Trends Driving Corporate Climate Strategies in 2024
Research firm Verdantix recently published a study surveying 353 global decision-makers, across 38 countries, on the key trends shaping their corporate climate change strategies in 2024. Currently, net zero targets cover a majority (92%) of global GDP. According to the study, prioritizing compliance, seeking competitive advantage, and aligning with stakeholder requirements are the top three […]
-
Celebrating Earth Day, Today and Everyday
We are proud to celebrate Earth Day, today and everyday, in our mission of preparing today’s buildings to meet tomorrow’s challenges. Historically, achieving a balance between building user comfort and experience resulted in increased energy consumption and cost, presenting a significant trade-off for building owners and operators aiming for efficiency and sustainability. R-Zero solutions remove […]
-
Creating Energy-Efficient Outcomes for Your Buildings
Q&A with R-Zero’s Matt Arneson In honor of Earth Month, we sat down with our in-house expert in energy efficiency, Matt Arneson, to learn more about how customers can drive sustainable outcomes across their buildings. Climate disclosure regulations, both domestic and international, seem to be in the news every week. Are building developers, owners, and […]
-
A Conversation with FEA President and COO Laurie Gilmer on Effective Facility Management
R-Zero recently connected with Laurie Gilmer, President and COO at Facility Engineering Associates (FEA) and former chair of the International Facility Management Association (IFMA), to discuss actionable ways that facility managers can improve their building performance and increase their energy savings. Through her work at the FEA, Laurie mentors facility managers on strategies to best […]
-
Finding Your Fit in the Sensing Maturity Model
The way we do business changes quickly, but the spaces in which we conduct that business do not. Hybrid work models, changing workforce preferences, operational priorities, and rising energy costs, have all fundamentally changed the way we use and think about our buildings and our workspaces. Thankfully, sensing technologies offer an easy and accessible solution […]
-
How Sensing Technologies Can Make Buildings More Responsive
Did you miss our most recent webinar on the five ways sensing technologies can make buildings healthier and more productive? In this session, R-Zero’s Vice President of Product Marketing, Uri Kogan, explores how implementing a broad sensor program that captures presence detection, occupant count, air quality, and environmental quality monitoring can be an effective tool […]
-
Customer Spotlight: Providing Usage Data to Corporate Real Estate Customers
Commercial companies know the importance of data; data insights allow them to optimize and adjust resources in order to achieve their long-term goals. That’s why savvy commercial companies seek out data about their employees’ workspace usage, in order to optimize their spaces for employee satisfaction and performance. R-Zero’s WorkPoint Sensors and WorkSpace Counters are developed […]
-
3 Strategies to Cut Energy and Operating Costs
If you missed R-Zero’s recent webinar on strategies to cut down on energy and operating costs, here’s a quick recap that covers our three main strategies for measuring, optimizing, and restructuring your building for maximum savings. Energy Usage in Buildings Commercial buildings spend a significant amount of money on energy, but the usage depends on […]
-
Navigating the Rising Costs of Meeting Building Ventilation and IAQ Standards
Building owners and operators have been faced with a threefold challenge of increasing costs to meet ventilation and indoor air quality standards in recent years. The three key drivers that contribute to the rising cost are: the increase in required indoor air quality standards, the cost increases in HVAC systems and labor, and the cost […]
-
Understanding Hospital Energy Usage
Healthcare buildings are energy-intensive structures, but none are more energy-intensive than hospitals. On average, hospitals use about 2.75 times the energy per square foot of all commercial buildings. Here’s a breakdown of what makes up a hospital’s large demand for energy, and how that energy demand can vary depending on the region. Hospital Energy Statistics […]
-
What is Upper-Room Ultraviolet Germicidal Irradiation (UVGI)?
Ultraviolet Germicidal Irradiation (UVGI) is a type of UV light used in hospitals and labs since the 1800s to effectively disinfect occupied spaces. It is a type of UV light similar to far-UV light, which we discussed in our last post, but with a few different properties and uses. As UVGI becomes more accessible for […]
-
What is Far-UV?
With ASHRAE’s new standards for maintaining clean indoor air, UV-C light is quickly becoming a leading method in deactivating microorganisms effectively and affordably. Constantly running an HVAC system to cycle in clean air has significant energy and financial costs, but cleaning the air in place with the power of UV-C light has the same effect […]
-
Debunking the myths about Ozone and UV-C
It’s natural to be concerned about the impact of ozone on human health and ask if a particular technology creates risk. But to make the right choice, it’s important to distinguish facts from fears. Below, we explain ozone production in various products, the link between Far-UV light and ozone, and how California’s stringent standards protect […]
-
What is Germicidal Ultraviolet-C (UVC) Light?
If you’ve been looking into safe and sustainable disinfection methods for your building, you’ve probably heard about germicidal ultraviolet-C light. But what is germicidal ultraviolet-C light, and what can it do to reduce microbial loads that increase the risk of infection or illness spreading? To answer that question, we’re going to have to start by […]
-
Don’t Miss R-Zero at Greenbuild This Year!
Greenbuild 2023 is all about building transformation, and you don’t want to miss the chance to talk with R-Zero about how we’re transforming the field of safer indoor air. Here’s where you can find us at the conference: Hear Our CEO Speak Our CEO, Jennifer Nuckles, will be hosting the “Revolutionizing Sanitation: Harnessing the Power […]
-
ASHRAE Announces Groundbreaking Standard to Improve Indoor Air Quality
The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) recently approved groundbreaking new guidelines, ASHRAE Standard 241, to reduce the risk of disease transmission in indoor spaces. This standard is a breakthrough in public health and has the potential to drastically reduce the spread of contagious illnesses in places like schools, office buildings, and […]
-
Sustainability In Practice—Using Utilization Data to Calculate Energy and Emissions Reduction Opportunities
Carbon reduction and energy efficiency are subjects we care deeply about at R-Zero. We want to help break down the silos that occupancy data traditionally resides in and apply it toward initiatives that are meaningful for the entire business. As such, we have built some basic calculations that can help organizations understand their emissions and […]
-
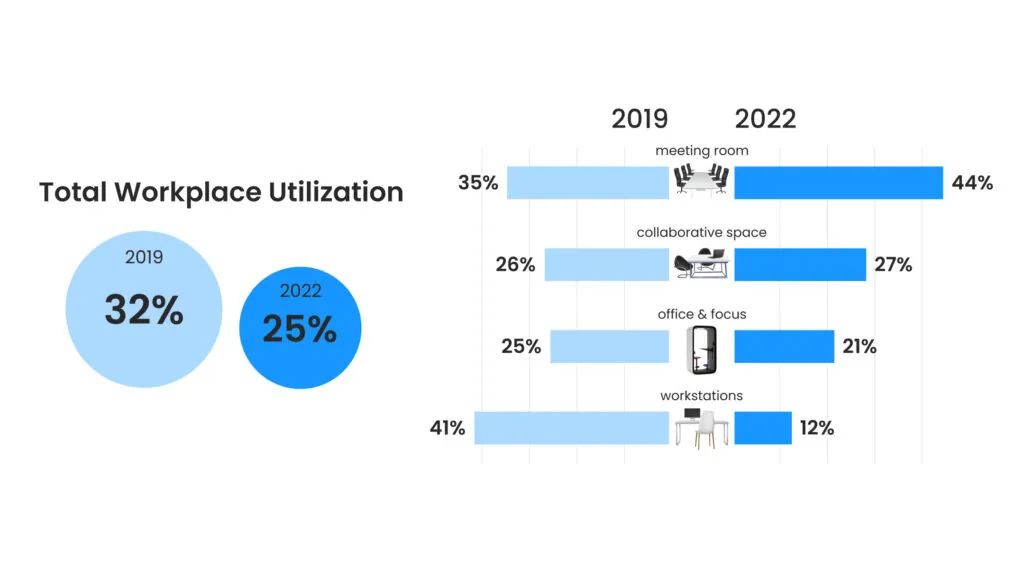
2022 Benchmark Data. Who Is Measuring What?
Hello Friends, Who ended 2022 where you thought you would? Well, many of our customers did not and some ended the year finding themselves in the middle of surprising new trends. We’d like to share with you some of our 2022 sensor-based Utilization Benchmark Data. If you are curious about any of these key findings, […]
-
Right-Sizing your Portfolio with Peak Metrics
A new way of working is here to stay. What started as a pandemic-era necessity has rapidly become the norm in many industries, including many fortune 500 companies and global corporations. Studies have shown that 73% percent of employees say they need a better reason to go into the office than just company expectations. It’s […]
-
Top 8 Essential Office Space Utilization Metrics & Their Applications
One thing we know for sure is that the future is uncertain. Instead of being stuck in a daze of wonder, real estate professionals are grounding their planning processes in data. So long as they have data to guide them, they can plan for hybrid work environments that are bound to change over time. Fortune […]
-
Allocation vs Utilization: Put Your Data in Action With Workplace Analytics!
If you’re a facility manager or otherwise deal with the business of organizing your office’s space, there are two terms you need to be familiar with: allocation and utilization. These terms are often used interchangeably, but they actually refer to very specific yet equally important aspects of creating a cost-effective and space-efficient workplace environment. Learning […]
-
Shining a New Light on the Spread of Coronavirus in the Classroom with UVC Disinfectant Solutions.
As cases spike in LA County and Southern California, do current coronavirus measures cause major disruption for students, teachers, and lesson plans, what are the proactive alternatives school districts should take to prepare for the next outbreak? Southern California’s COVID Tipping Point Since late October, LA County’s coronavirus case rate has tripled with a reported […]
-
Improving Texas Schools with TEA Funds
Furthering hands-on developmental learning – with indoor safety. Safer indoor, in-person learning with TEA Funds As the world began to return to in-person activities, and organizations started leading their teams back to in-office environments, schools worldwide knew that returning in-person was necessary for hands-on collaboration and more engaging educational experiences. But how were educational facility […]
-
Step up to the Challenge: Cleaner Air in Buildings
How to Improve Indoor Air Quality Plus the Innovations Needed to Remediate Concerns. Indoor Air Quality Standards are now Higher than Ever Collectively, we all measure the health of the water we drink on a daily basis and the outdoor air pollutants that affect our breathing everyday, but why has indoor air quality been an […]
-
3-30-300 Rule and ROI
When it comes to selling a product, ROI is easy to visualize by simply comparing expenditure to profit—but what about estimating returns on your actual workspace? Office space is a company’s second largest cost behind people, and managers tasked with improving workplace utilization often have little reference for what drives productivity and thus makes workspace […]
-
R-Zero Named to Forbes’ 2022 Next Billion-Dollar Startups List
As humans, we spend 90% of our lives indoors. Yet for decades, the built environment has been optimized for energy efficiency, instead of people. And while society has made strides in ensuring the water we drink and the food we eat is safe — the indoor air we breathe 18-20,000 times per day has long […]
-
Office Layout Ideas: How to Design Hybrid Office Space
With most American companies still in the throes of what RTO means to them, now is an opportunity for owners, operators, and tenants to reinvent the kind of space their workforce will be working in for the coming years. The pandemic has presented the business world with the opportunity to take part in the Great […]
-
Senior Care Facilities Need the Healthy Buildings Movement
Since the announcement by the Biden administration focusing on clean air in buildings as part of their National Covid Strategy, interest in the Healthy Buildings movement has picked up momentum. The growing understanding of the need for buildings to provide more than shelter for businesses and families is becoming a topic of frequent conversation. From […]
-
How the Pandemic Positioned Healthy Buildings as a Public Health Imperative
Discussions about healthy buildings are becoming increasingly relevant in conversations about changes brought on by the COVID-19 pandemic. Throughout history, wars, famines, plagues, and natural disasters have all challenged the human species. At every turn, humans have proven their adaptability, problem-solving abilities, and determination not only to survive but to grow, learn, and emerge better […]
-
New Work Schedules With the 3/2 Split (3 in Office, 2 at Home)
The Covid-19 pandemic forced the introduction of plenty of creative solutions to coworking in the lockdown era. Almost overnight, and with literal lives on the line, companies around the world had to fundamentally change the way they did business to accommodate social distancing protocols and quarantines. Two years on, many businesses have grown accustomed to […]
-
A Hybrid Office for Everyone
When the Covid-19 pandemic spread to the mainland United States in March of 2020, unbeknownst to the public, a huge scale experiment in altering the layout of the American business culture was about to begin. With nationwide quarantine orders in effect, businesses spent billions investing in Work From Home infrastructure—including things like altered scheduling, teleconference, […]
-
How Workplace Environment Affects Employee Productivity
It’s the basic question that every manager or business owner needs to answer: “What can I do to help my employees be more productive?” However, recent studies have shown that question may already be answered by the time your employees first set foot in their workspace. Factors like temperature, lighting, and noise can have a […]
-
R-Zero’s Jeff Wagner on the Built Environment & People
R-Zero is proud to announce that built environment expert Jeff Wagner, former Chief of Facilities for Clark County School District in Nevada, has joined the team as General Manager of Education. As a trained architect and former college professor, Jeff brings a wealth of experience regarding the impact of the built environment on people-performance. Before […]
-
Protecting Personal Information Privacy: Anonymous Workspace Occupancy Sensors Instead of Cameras
The right to privacy in the workplace has become a hot-button legal and ethical issue. As technology evolves to better automate, codify, and streamline our work, so do the increasingly intrusive methods by which our lives are monitored—both online in the real world. Detailed information about the workplace is invaluable for it’s cost-saving applications, but […]
-
Improving Employee Efficiency with Meeting Room Occupancy Sensors
No matter how much employers or building managers wish there was a magic formula for improving employee efficiency, it remains a complex problem that depends on a lot of factors. issues with scheduling, space management, and even office comfort levels all directly influence the quality of work your employees are capable of. When confronting an […]
-
R-Zero vs Density: Differences That Will Guide You to Make a Final Decision
Investing in the new generation of smart office technology can sometimes feel like a leap of faith, especially when you don’t know what systems will work best for your unique business environment. Occupancy sensors for offices can provide crucial data about how your office or workplace is actually used by employees—data which can translate to […]
-
Sensor Data Collection and Employee Privacy
As the role of digital technology in the workplace has grown exponentially over the past two decades, so has the need for oversight of what information is collected by digital services used by employers. A Pew Research survey on consumer privacy found that “93% of adults say that being in control of who can get […]
-
Cleaning and Disinfecting with Chemicals: What to Know
Cleaning and disinfecting with chemicals such as bleach have been go-to methods since the start of the last century. Chemical products are often inexpensive and convenient cleaners used in organizations, public facilities, and people’s homes. Recently, bleach and other chemical disinfection methods have been an integral part of disinfecting surfaces during the pandemic, helping curb […]
-
R-Zero Acquires CoWorkr to Advance Indoor Health and Productivity
By Grant Morgan, Co-Founder In the introduction to their influential 2020 book Healthy Buildings: How Indoor Spaces Drive Performance and Productivity, Joseph G. Allen and John D. Macomber describe the multidisciplinary pursuit of healthier indoor spaces as “the greatest untapped business and health opportunity of our time.” Today, R-Zero is significantly advancing the future of […]
-
Building a Modern Business with Occupancy Sensor Data
Going to the office isn’t like what it used to be. Instead of giant labyrinths of cubicles and meeting spaces, modern workspaces need to be flexible, and designed to meet employee demands. In the digital age, workplace management is really about data management, and that’s where R-Zero occupancy sensors can mean the difference between wasted […]
-
R-Zero’s Journey & Becoming Disinfection Technology Pioneers in 14 Months
By Grant Morgan, Co-Founder R-Zero is a company with an ambitious vision: to create a world without sick days. Today, while a global pandemic continues to claim lives and devastate economies, that vision seems particularly far fetched. But we see a hopeful future – one even better than what we knew before – and we will […]
-
Let the Data Be Your Guide: Understanding PreCOVID19 Data to Build Future Strategies
Since R-Zero’s first deployment study in 2014, we have collected over 6M days of data. This is an enormous amount of utilization information that represents a wide range of sectors like tech, pharma, financial, and more. This data represents a time in workplace occupancy that we may not be able to replicate for years to […]
-
Facilities Management Trends in 2021
Facilities Management is a crucial, and sometimes underappreciated, aspect of any business where an office or workspace is a necessity. Proper FM balances both employee experience with cost-balancing measures and is crucial to a comfortable, well-functioning workplace. In 2021, as businesses are returning to work but stay mindful of lessons learned during the pandemic, FM […]
-
How CANOPY is Creating a Healthy Return to Its Coworking Communities
Before the start of the COVID-19 pandemic, San Francisco was arguably the coworking capital of the U.S. In 2018, the city had more coworking spaces per capita than any other major city in the country. In San Francisco’s ecosystem of tech startups, entrepreneurs and creatives, coworking spaces have in recent years served as a preferred […]
-
WorkPlace Utilization: Discrepancies between CAFM, Badge, & Sensor Data
It’s not uncommon for an organization’s assumed workplace utilization to be vastly different from reality. We’ve found this to be due to several things— a lack of understanding in what utilization represents and the low fidelity of the tools used when measuring. Historic methods for determining utilization are not actually processes of measuring at all […]
-
Explaining the Types of Anonymous Occupancy Sensors
Passive infrared sensing devices have become ubiquitous in commercial real estate. The technology has become a standard in many applications due to its simple and completely anonymous method of detecting presence. Historically, building systems have utilized the integration of granular motion sensors and their basic occupancy event data for driving improvements in energy usage. Sensors […]
-
WorkPlace Data: Occupancy vs. Utilization
Not everyone analyzing workplace data has experience in workplace metrics and, even for professionals, there can be confusion when comparing occupancy to utilization. While the two are often used interchangeably, they are in fact very different. Think back to the days when companies would pay a person to walk through a building with a clipboard […]
-
Preserving Productivity with Healthy Workplaces
We’ve always considered workplace productivity the golden metric because it relates to growth, worker satisfaction, and retention. We have recently seen how digital tools can lead to time efficiency, continuity, and effectiveness while working from home. The area of productivity that real estate and facilities teams can have the most impact on is in the […]
-
A Safer Workplace is a Connected Workplace
There is a lot of confusion about real-time workplace data. When R-Zero talks real-time, we mean it. Our sensors update to the cloud instantaneously when a seat or space becomes occupied or vacated. Why is this important? Because real-time data will run the future office. Making data available to staff can alleviate fears and build […]
-
How Using Workplace Data can Decrease Janitorial Expenses for Your Business
While North American companies are depending on summertime heat to quell the virus and usher in the commencement of business, experts believe that this virus may be here to stay, returning each fall and winter, as an endemic seasonal concern. We all know that lockdown can’t go on forever, yet to ensure the safety and […]
-
How to Decrease Costs in a Business with Low Workplace Utilization
In the shadow of COVID-19, business strategists are finding themselves suddenly stranded in dark and uncharted territory. Struggling to reclaim and retain market stability under a nail-biting stock-market decline, businesses are seeing an en-mass clearing of desks as entire workforces are ordered into self-quarantine, to care for loved ones whilst trying to manage their work […]